More than just a job
My name is Susie, I am the founder and CEO of Telebehavioral Health.US. I founded the company in 2016. I have been a Clinical Social Worker since graduating from Grand Valley State University with my Master's Degree in 2004. My career in social work consisted of long hours that regularly extended into the evenings and included numerous “side gigs,” to make a sustainable living. Whether I was teaching classes at a local university, providing on-call case management with an insurance company, facilitating speaking engagements or professional development courses, or moonlighting as a clinical supervisor, I was left with less and less time with, and for, my children. Putting food on the table and a roof over our heads was necessary, having time with my children was a luxury. I love being a social worker and like most social workers will tell you being a social worker is more than a job or career, it is a calling. Unfortunately the field does not leave much room for life outside of social work.

A workforce crisis
Social workers are one of the largest groups of professional Mental Health and Substance Use service providers in the United States. The lifetime burnout rate for social workers is 75%. Systemic reviews of this industry have identified the “biggest indicator of burnout to be the stressful workforce environment.” Ironically, the mental health field has paid relatively little attention to the health and well-being of its own workers. (NIMH)” In 2019, The Office Group published a comparison of industry "burnout" and found “when compared to all other industries Social Workers are most likely to suffer from work-related stress, depression and anxiety.”
The national annual median salary for a Master of Social Work is an average of $20k less than their non-social work counterparts with similar levels of education and experience. In addition to the salary gap, social workers are expected to work long and typically non-traditional hours, in often unsafe working conditions. They are consistently exposed to vicarious and secondary trauma and frequently experience wage freezes in the nonprofit sector.
A female dominated field
Eighty percent of social workers are women. Women are more likely to also bear the responsibility of what sociologist Arlie Hochschild identified as “the second shift.” These duties consist of unpaid tasks around the house such as meal preparation, housekeeping, home economics, and care taking of others in the home. In the field of social work, there is very little opportunity for workers to set their own hours and productivity standards. Production standards are also frequently increasing and constantly changing depending on program funding. For this female dominated workforce these industry conditions exacerbate a massive provider shortage for the leading source of disease burden in the United States (SAMHSA).

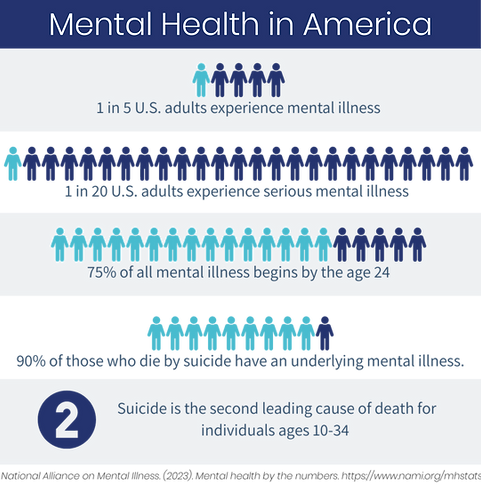
A leading source of disease burden
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), mental illness is "the leading source of disease burden in the United States." Over the past few years suicide has gone from being the second leading cause of death for Americans ages 14-24 years old to the second leading cause of death for 10-34 years old. "Deaths of Despair" are a thing, and they are on the rise in the midst of a massive opioid crisis. At the same time, over the past two decades, the United States has had a growing Mental Health Provider Shortage with 40 Million Americans who need treatment each year not having access to it. The shortage is so immense that Congress refers to it as a “workforce crisis.” 111 million Americans live in Federally Designated Mental Health Provider Shortage Areas (MHPSA). Prior to the Covid-19 pandemic the behavioral health workforce was expected to have a provider shortage estimated to be 250,000 workers short of the projected need by the year 2025.
A call to action
Over the past decade, the National Institute of Mental Health, The Substance Abuse and Mental Health Services Administration, the American Medical Association, the American Psychological Association, and the American Telemedicine Association have engaged in a national call to action for mental health and substance use providers to utilize telemedicine through a nationally supported “Direct to Consumer” model of care. Since 2016 The Health Resources and Services Administration has been reporting, to anyone who would listen, how "the unmet need in mental health care was too large to be addressed without leveraging technological innovations." This call to action was heard, just not by providers. Unfortunately software developers were listening. In the same time frame, numerous platform-based companies advertising "on-line therapy," "e- counseling," and "web-therapy," have raked in a combined estimated annual revenue of over $500 million by licensing their platform to almost 10,000 therapists in the United States. All having absolutely no impact on the disease burden or provider shortage, they both have only gotten worse, and here is why.

Is it the same "therapy?"
As consumers, we are led to believe these platform-based companies are “healthcare organizations,” and are legitimately providing telemedicine or telemental health services, but they are not. Websites like MDLive, Talkspace, Betterhelp, Insight+Regroup, AmWell, Teledoc, AbleTo and Open Path Psychotherapy Collective are not healthcare organizations, they are software companies providing the platform. Telemedicine, by definition, requires the same procedure or service that would be provided in a brick and mortar setting, be delivered using a secure telecommunications platform. It must be the same service.
The services offered by these software companies do not meet the definition of telemedicine and they are not providing actual therapy. While on the front end of their websites, every single one of them claims the are providing a health service, each of them has back-end disclaimers referring to their services as "for informational purposes only, how services are “not a replacement for therapy,” their organization is "not a healthcare provider" and how their therapist will not diagnose, provide recommendations or provide treatment. Diagnosis, planning and providing treatment are the main tenets of therapy and why therapy works. Furthermore, therapy also "works," because of privacy and confidentiality laws required by the Federal Government, these laws include HIPAA and HITECH, which these companies are not regulated under, because they are software companies and not healthcare organizations. You will find in almost every single one of their disclaimers a statement identifying they are not legally bound to these laws that protect your healthcare confidentiality.
Perhaps the most concerning and egregious common practice of these companies is the lack of oversight they provide to the almost 10,000 clinicians they contract with. Each one also has a disclaimer explaining how there is no oversight of the services being provided and how the company has no relationship with the therapists providing the services. Not providing oversight of clinical services creates a level of risk that is not acceptable in healthcare and puts vulnerable populations at greater risk.

The solution
The solution is not in duping consumers into thinking licensed platforms sold by software companies are providing telemedicine services. It isn't even that complex. In order to address the leading source of disease burden and national workforce crisis we have to start addressing the specific workforce conditions and needs of this female dominated profession by creating opportunities for higher wages and more flexible hours. Right now, many of us are celebrating how telemedicine expands the reach of services, reduces barriers, saves time, saves money, helps those with transportation problems and in light of the national pandemic keeps clients and providers safe. What many don't realize is that telemedicine also provides an opportunity for higher pay and more flexible hours for mental health providers.
TelebehavioralHealth.US
In September of 2016, just a few months after Michigan expanded telehealth to include social workers, I left my brick-and-mortar practice and opened the first telemedicine behavioral health practice in Michigan. My goal was to increase access for those in Mental Health Provider Shortage Areas while also addressing the provider shortage by creating opportunities that improve workforce conditions and address the specific needs of a female-dominated workforce. I wanted to create a business and practice model based on one main tenet: taking care of the providers' needs so they can provide care to those in need.
I started the company on my own with no investment, other than my own "sweat equity." I carried a low volume of patients and scraped by financially so I could build the practice in a way that felt like building a sandcastle, one grain of sand at a time. I was one of the first providers in the country to adopt the American Telemedicine Association and American Psychological Association's "Direct to Consumer" model using a Video Telecommunications Platform. Being the first meant forging a lot of new territory with payers and consumers. For starters, when I started, there was no one to assure me that I would be able to get reimbursed; telehealth was such an unknown. I would spend hours on the phone with insurance company service reps who had never heard of anyone doing what I was trying to do, resulting in unbearably slow reimbursement. I remember a time, two years after I started the practice, when I received a monthly newsletter from United Behavioral Health, announcing to Licensed Clinical Social Workers that we could "now start billing for telebehavioral health services." United had been reimbursing me for telebehavioral health for almost two years.

What we have learned so far
Maslow teaches us about how we have a hierarchy of needs and if our basic physical, social, and emotional needs are not being met, we can not self actualize and live our true potential. We can not keep requiring this workforce to earn a high level of education only to be underpaid and overworked and not expect consequences such as having mental illness be the leading source of disease burden. We have to take care of our workforces that service our vulnerable populations including our female dominated ones.
And to my fellow social workers. Please, for the love of all that is mighty, PLEASE, when "they" tell you becoming a social worker means you will, "make no money," do not respond by saying this is essentially, "okay" because you are "called to do it." I am here to tell you, you are in demand, your services are valued and you deserve to earn an income that matches your education and experience that doesn’t conflict with the other important roles in your life. Mostly, I am here to say, we would love to have you join our movement.
Warmest regards,
Susie Rigas-Morozowich, LMSW, LCSW
Co-Founder and CEO
TelebehavioralHealth.US

Ready to Get Started?
We provide online therapy with licensed clinicians. Insurance is accepted, and you can schedule your first appointment online in just a few minutes.


